Bone platform switching involves an inward bone ring in the coronal part of the implant that is fitting with the alveolar bone crest.
The concept of platform switching was developed to control bone loss after implant placement. ‘Platform switching’ refers to the use of an abutment of a smaller diameter that is connected to an implant neck with a larger diameter; this connection shifts the perimeter of the implant-abutment junction (IAJ) inward, toward the central axis (the middle of the implant), in order to improve the force distribution.
Quirynen et al. [1] suggest that bacterial leakage occurs through the micro gap of the junction;
IAJ. Ericsson et al. [2] found histologic evidence that an inflammatory cell infiltration is located 1 to 1.5 mm adjacent to the IAJ after implant placement. To protect the underlying bone from this inflammatory cell infiltration and microbiologic invasion, 1 mm of healthy connective tissue is needed to establish a biologic seal comparable to that around natural teeth [2,3].
This movement of the IAJ is also believed to shift inflammatory cell infiltration to the central axis of the implant and away from the adjacent crestal bone, which is thought to restrict crestal bone reabsorption [4].
Indeed, Hurzeler et al. [5] reported that the concept of platform switching does appear to limit crystal reabsorption and preserve the peri-implant bone level.
They found that in the platform-switching group, the amount of bone loss was significantly lower than in the control group.
Bone platform switching involves an inward bone ring in the coronal part of the implant that is fitting with the alveolar bone
crest. The concept of platform switching was developed to control bone loss after implant placement. ‘Platform switching’
refers to the use of an abutment of a smaller diameter that is connected to an implant neck with a larger diameter; this
connection shifts the perimeter of the implant-abutment junction (IAJ) inward, toward the central axis
(the middle of the implant), in order to improve the force distribution.
Quirynen et al. [1] suggest that bacterial leakage occurs through the micro gap of the junction;
IAJ. Ericsson et al. [2] found histologic evidence that an inflammatory cell infiltration is located 1 to 1.5 mm adjacent to the IAJ
after implant placement.
To protect the underlying bone from this inflammatory cell infiltration and microbiologic invasion, 1 mm of healthy connective tissue is needed to establish a biologic seal comparable to that around natural teeth [2,3].
This movement of the IAJ is also believed to shift inflammatory cell infiltration to the central axis of the implant and away from the adjacent crestal bone, which is thought to restrict crestal bone reabsorption [4].
Indeed, Hurzeler et al. [5] reported that the concept of platform switching does appear to limit crystal reabsorption and preserve the peri-implant bone level.
They found that in the platform-switching group, the amount of bone loss was significantly lower than in the control group.
Lopez-Mari et al. [6] found that platform switching is capable of reducing or eliminating crestal bone loss up to 1.56±0.70 mm. Additionally, it appears to help maintain the width and height of crestal bone and the crestal peak between adjacent implants and reduces circumferential bone loss. It was concluded that the implant design modifications involved in platform switching offer multiple advantages and potential applications, including situations in which a larger implant is desirable but the prosthetic space is limited, and in cases when some implants are desirable in the anterior zone where preservation of the crestal bone can lead to improved aesthetics.
From a review of the literature, Kwon et al. [7] concluded that the marginal bone loss associated with a flat-top implant is 1.0 to 1.3 mm at one year post-implantation, even in the presence of an improved surface [8–10]. In contrast, the marginal bone loss with a microthread, conical seal, and platform-switched design was found to be 0.11 to 0.24 mm [11,12].
The authors concluded that the marginal bone levels of the subjects in their study (0.16 to 0.17 mm) were comparable to those of previous studies. Similarly, in the present study, the mean amount of marginal bone loss was smaller, and it can therefore be assumed that micro-threaded and platform-switched implants are capable of reducing marginal bone loss due to specific features in the implant design.
References
1. Quirynen M, Bollen CM, Eyssen H, van Steenberghe D. Microbial penetration along the implant components of the Brånemark system. An in vitro study. Clin Oral Implants Res. 1994;5:239–244.[PubMed]
2. Ericsson I, Persson LG, Berglundh T, Marinello CP, Lindhe J, Klinge B. Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol. 1995;22:255–261. [PubMed]
3. Waerhaug J. Subgingival plaque and loss of attachment in periodontosis as evaluated on extracted teeth. J Periodontol. 1977;48:125–130. [PubMed]
4. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26:9–17. [PubMed]
5. Hürzeler M, Fickl S, Zuhr O, Wachtel HC. Peri-implant bone level around implants with platform-switched abutments: preliminary data from a prospective study. J Oral Maxillofac Surg. 2007;65(7 Suppl 1):33–39. [PubMed]
6. López-Marí L, Calvo-Guirado JL, Martín-Castellote B, Gomez-Moreno G, López-Marí M. Implant platform switching concept: an updated review. Med Oral Patol Oral Cir Bucal. 2009;14:e450–e454.[PubMed]
7. Kwon HJ, Lee DW, Park KH, Kim CK, Moon IS. Influence of the tooth- and implant-side marginal bone level on the interproximal papilla dimension in a single implant with a microthread, conical seal, and platform-switched design. J Periodontol. 2009;80:1541–1547. [PubMed]
8. Calandriello R, Tomatis M, Vallone R, Rangert B, Gottlow J. Immediate occlusal loading of single lower molars using Brånemark System Wide-Platform TiUnite implants: an interim report of a prospective open-ended clinical multicenter study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):74–80.[PubMed]
9. Glauser R, Lundgren AK, Gottlow J, Sennerby L, Portmann M, Ruhstaller P, et al. Immediate occlusal loading of Brånemark TiUnite implants placed predominantly in soft bone: 1-year results of a prospective clinical study. Clin Implant Dent Relat Res. 2003;5(Suppl 1):47–56. [PubMed]
10. Vanden Bogaerde L, Pedretti G, Dellacasa P, Mozzati M, Rangert B, Wendelhag I. Early function of splinted implants in maxillas and posterior mandibles, using Brånemark System Tiunite implants: an 18-month prospective clinical multicenter study. Clin Implant Dent Relat Res. 2004;6:121–129. [PubMed]
11. Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J. Implant-supported single-tooth restorations: a 5-year prospective study. J Clin Periodontol. 2005;32:567–574. [PubMed]
12. Lee DW, Choi YS, Park KH, Kim CS, Moon IS. Effect of microthread on the maintenance of marginal bone level: a 3-year prospective study. Clin Oral Implants Res. 2007;18:465–470. [PubMed]
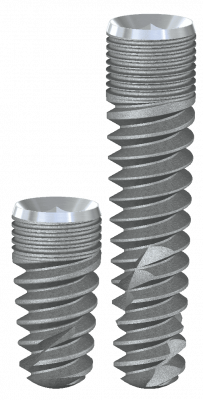

The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease. The enhanced
deep thread simplifies the insertion and allows
for high primary stability.
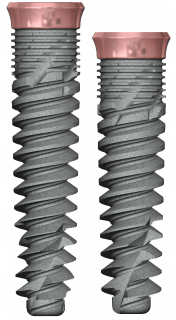
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease. The enhanced
deep thread simplifies the insertion and allows
for high primary stability.
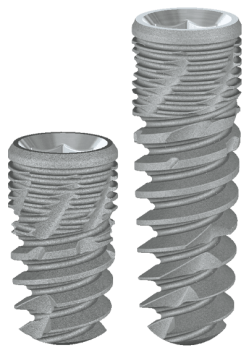
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease. The enhanced deep thread simplifies the insertion and allows for high primary stability.
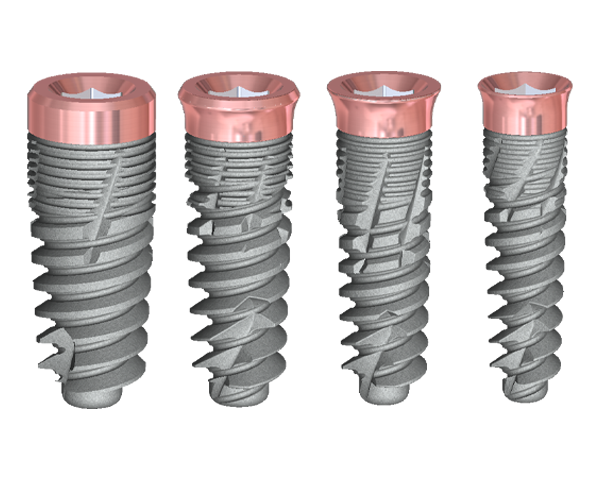
The pink tissue versatile implant neck combines superior gingival aesthetics and high primary stability, improved placement, and temporization, which is particularly beneficial in aesthetically demanding cases.