Bone healing after implantation
Bone healing after implantation
A successful implantation process is complete when the implant is safely secured to the bone, and functioning within the bone framework. In the past a special bone cement was used to “glue” the implant to the bone [1]; however, presently implants are manufactured in a way that allows the host bone to heal around the implant, securing it to its place [2]. This process is called “osseointegration”, or bone-bonding [3].
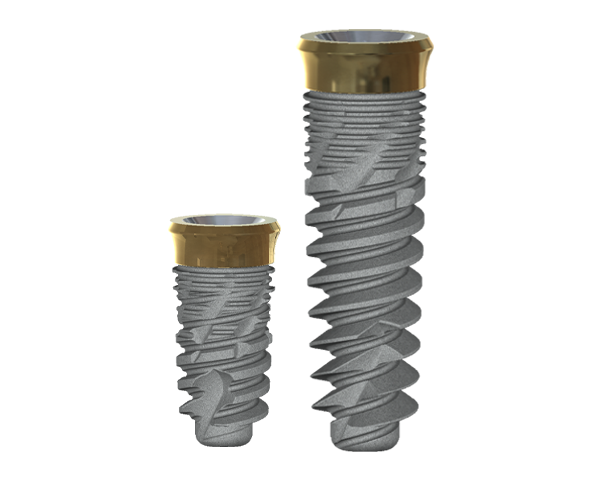
Bones are constantly remodeling, meaning that the bone disassembles and rebuilds itself; therefore, the implant’s surface must have specific surface topographies, containing pores and complex 3D characteristics, for the bone to bond to the implant surface [2]. This results in implant integration.
This is a short summary of the peri-implant bone healing process:
Primary implant fixation:
The implant must be securely fixed to the host bone to ensure proper healing, allowing bone formation without causing too much movement [4,5]. Just as in the case of a fracture, wherein movement between broken edges of the fractured bone may impede the healing process [6-8], osseointegration is inhibited when the implant is not adequately secured to the bone [9]. There is a delicate balance to implant placement, however, because a certain degree of space is required between the implant and the host bone for the bone to form properly [10,11].
Blood-implant contact:
The implantation process begins with a surgical procedure, which leads to bleeding from the soft tissues surrounding the bone and ultimately, to the formation of a hematoma. The contact of blood and the foreign object – the implant – results in various biological processes, such as inflammation, coagulation, and tissue formation, which are influenced by the surface chemistry and topography of the implant [12]. These processes create a monolayer of proteins, such as fibronectin and vitronectin, which can attach to the implant’s surface and interact with it, if the topography and chemistry of the implant are conducive to acceptance by the body [13,14]. These interactions between the implant and the proteinous monolayer create the basis for osseointegration and ossification (bone formation) and are crucial to the proper healing of the wound and, ultimately, successful implantation.
Platelet activation and coagulation:
The first step towards healing is blood coagulation around the implant, which is controlled by the platelets [15]. Platelets are small cells that are activated by foreign objects, injured tissues, or signals released from other cells. Upon activation, the platelets secrete various molecules that interact with coagulation factors and begin the coagulation process [16], and express adhesion receptors that enable platelet-implant interaction [17]. These processes result in the formation of a clot [18, which will provide the conditions necessary for osteoconduction (recruitment of bone cells) [19]. The variety of cytokines, growth factors and chemoattractants the clot contains encourage cell migration and adhesion [20-22].
The surface topography, as mentioned earlier, is one of the key factors in the success of these initial stages of bone formation. Studies have shown that roughened implant surfaces with nano-and-micro-topography display better activation than smooth surfaces [23]. Considering the importance of clot formation to the migration of cells towards the implant and to the inflammation and osteoconduction processes, it is easy to understand why surface topography and chemistry can have a great influence on successful healing [24,25].
Inflammation and angiogenesis:
The inflammatory response begins immediately following activation of the platelets and the coagulation process [16]. Immune cells arrive to the transplant area and trigger the release of cytokines [26]. These cytokines encourage inflammation, and appear to contribute to bone formation by inducing recruitment or maturation of bone cells [27]. Apart from the cytokines, another family of factors, called tissue growth factors β (TGF- β), are secreted; these factors further promote the formation on new bone, and improve healing of fractures and implantation wounds [28-33].
Bone cells, like all body cells, require consistent blood supply; therefore, angiogenesis (formation of new blood vessels) is crucial to the implant process, and angiogenic factors, such as VEGF, are secreted to induce new blood vessel growth [34-36].
The result of the inflammatory and engionenic processes is attraction and activation of bone cells, thereby creating the conditions needed for the formation of new bone around the implant.
Bone formation:
Attracted by the signaling molecules secreted in the area of the wound, mesenchymal cells arrive and differentiate into bone-building cells (osteoblasts) that begin to secrete matrix [37,38]. This matrix serves as cement, as well as a site for mineralization [39-41], so a calcified layer can be formed on the implant surface. This layer grows and expands, and the immature bone is then formed toward the implant and the surrounding tissues [42]. The growing immature bone also provides additional support to the implant [43]. After the wound is healed, the primary layer of bone on the implant surface dies and is absorbed, and the implant is anchored by bonding to the mature bone and the implant surface. If the implant surface features multi-dimensional complex topography then the bone can easily integrate into its surface, as opposed to smooth surfaces, where the bone simply grows around the implant [44]. If successful, the bone formation process ends with a strong fixation of the implant to the bone.
In summary, implantation triggers a cascade of events, starting with the formation of a hematoma, secretion of various factors, activation of platelets, and clot formation. This is followed by the arrival of immune cells, which induce inflammation. Later on, angiogenesis occurs, blood vessels grow toward the implant, and bone cells become mature and begin building the new bone. This results in a primary, immature bone formation on the implant surface, which is later on replaced by a mature bone. When the process is completed successfully, the implant is securely fixed in the host bone and functions as a natural extension of it.
References:
1. Charnley J. Arthroplasty of the hip: A new operation. Lancet. 1961;1:1129–32. [PubMed: 15898154]
2. Davies JE. Bone bonding at natural and biomaterial surfaces. Biomaterials. 2007;28:5058–67. [PubMed: 17697711]
3. Marco F, Milena F, Gianluca G, Vittoria O. Peri-implant osteogenesis in health and osteoporosis. Micron. 2005;36:630–44. [PubMed: 16182543]
4. Cameron HU, Pilliar RM, MacNab I. The effect of movement on the bonding of porous metal to bone. J Biomed Mater Res. 1973;7:301–11. [PubMed: 4737675]
5. Franchi M, Fini M, Martini D, Orsini E, Leonardi L, Ruggeri A, et al. Biological fixation of endosseous implants. Micron. 2005;36:665–71. [PubMed: 16233979]
6. Cullinane DM, Fredrick A, Eisenberg SR, Pacicca D, Elman MV, Lee C, et al. Induction of a neoarthrosis by precisely controlled motion in an experimental mid-femoral defect. J Orthop Res. 2002;20:579–86. [PubMed: 12038634]
7. Gerstenfeld LC, Cullinane DM, Barnes GL, Graves DT, Einhorn TA. Fracture healing as a post-natal developmental process: Molecular, spatial, and temporal aspects of its regulation. J Cell Biochem. 2003;88:873–84. [PubMed: 12616527]
8. Le AX, Miclau T, Hu D, Helms JA. Molecular aspects of healing in stabilized and non-stabilized fractures. J Orthop Res. 2001;19:78–84. [PubMed: 11332624]
9. Pilliar RM, Lee JM, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res.1986;208:108–13. [PubMed: 3720113]
10. Goodman S, Aspenberg P. Effects of mechanical stimulation on the differentiation of hard tissues. Biomaterials. 1993;14:563–9. [PubMed: 8399946]
11. Futami T, Fujii N, Ohnishi H, Taguchi N, Kusakari H, Ohshima H, et al. Response to titanium implants in the rat maxilla: Ultrastructural and histochemical observations of the bone-titanium interface. J Periodontology. 2000;71:287–98.
12. Puleo DA, Nanci A. Understanding and controlling the bone implant interface. Biomaterials. 1999;20:2311–21. [PubMed: 10614937]
13. Ratner BD. New ideas in biomaterials science: A path to engineered biomaterials. J Biomed Mater Res. 1993;27:837–50. [PubMed: 8360211]
14. Kieswetter K, Schwartz Z, Dean DD, Boyan BD. The role of implant surface characteristics in the healing of bone. Crit Rev Oral Biol Med. 1996;7:329–45.[PubMed: 8986395]
15. Kanagaraja S, Lundström I, Nygren H, Tengvall P. Platelet binding and protein adsorption to titanium and gold after short time exposure to heparinized plasma and whole blood. Biomaterials. 1996;17:2225–32. [PubMed: 8968516]
16. Gorbet MB, Sefton MV. Biomaterial-associated thrombosis: Roles of coagulation factors, complement, platelets and leukocytes. Biomaterials. 2004;25:5681–703. [PubMed: 15147815]
17. Hanson SR. Blood coagulation and blood-material interations. In: Ratner RD, Hoffman A, Schoen F, Lemons J, editors. Biomaterials Science. 2nd ed. San Diego, CA: Academic Press; 2005. pp. 332–8.
18. Davies JE, Hosseini MM. Hosseini MM. Histodynamics of endosseous wound healing. In: Davies JE, editor. Bone Engineering. Toronto, ON: Em squared inc; 2000. pp. 1–14.
19. Anderson JM. Blood Inflammation, wound healing and foreign body response. In: Ratner RD, Hoffman A, Schoen F, Lemons J, editors. Biomaterials Science.2nd ed. San Diego, CA: Academic Press; 2005. pp. 296–304.
20. Spisani S, Giuliani AL, Cavalletti T, Zaccarini M, Milani L, Gavioli R, et al. Modulation of neutrophil functions by activated platelet release factors.Inflammation. 1992;16:147–58. [PubMed: 1317360]21. Ammon C, Kreutz M, Rehli M, Krause SW, Andreesen R. Platelets induce monocyte differentiation in serum-free coculture. J Leukoc Biol. 1998;63:469–76.[PubMed: 9544577]
22. Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z, et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat Med. 2009;15:757–65. [PMCID: PMC2727637] [PubMed: 19584867]
23. Kikuchi L, Park JY, Victor C, Davies JE. Platelet interactions with calcium-phosphate-coated surfaces. Biomaterials. 2005;26:5285–95. [PubMed: 15814126]
24. Gruber R, Karreth F, Kandler B, Fuerst G, Rot A, Fischer MB, et al. Platelet-released supernatants increase migration and proliferation, and decrease osteogenic differentiation of bone marrow-derived mesenchymal progenitor cells under in vitro conditions. Platelets. 2004;15:29–35. [PubMed: 14985174]
25. Davies JE. Understanding peri-implant endosseous healing. J Dent Educ. 2003;67:932–49. [PubMed: 12959168]
26. Bazzoni G, Dejana E, Del Maschio A. Platelet-dependent modulation of neutrophil function. Pharmacol Res. 1992;26:269–972. [PubMed: 1437991]
27. Gerstenfeld LC, Cho TJ, Kon T, Aizawa T, Cruceta J, Graves BD, et al. Impaired intramembranous bone formation during bone repair in the absence of tumor necrosis factor-alpha signaling. Cells Tissues Organs. 2001;169:285–94. [PubMed: 11455125]
28. Einhorn TA. The science of fracture healing. J Orthop Trauma. 2005;19:S4–6. [PubMed: 16479221]
29. De Long WG, Jr, Einhorn TA, Koval K, McKee M, Smith W, Sanders R, et al. Bone grafts and bone graft substitutes in orthopedic trauma surgery. A critical analysis. J Bone Joint Surg Am. 2007;89:649–58. [PubMed: 17332116]
30. Sumner DR, Turner TM, Purchio AF, Gombotz WR, Urban RM, Galante JO. Enhancement of bone ingrowth by transforming growth factor-beta. J Bone Joint Surg Am. 1995;77:1135–47. [PubMed: 7642657]
31. Lin M, Overgaard S, Glerup H, Søballe K, Bünger C. Transforming growth factor-beta1 adsorbed to tricalciumphosphate coated implants increases peri-implant bone remodeling. Biomaterials. 2001;22:189–93. [PubMed: 11197493]
32. Liu Y, Huse RO, de Groot K, Buser D, Hunziker EB. Delivery mode and efficacy of BMP-2 in association with implants. J Dent Res. 2007;86:84–9.[PubMed: 17189469]
33. Park J, Lutz R, Felszeghy E, Wiltfang J, Nkenke E, Neukam FW, et al. The effect on bone regeneration of a liposomal vector to deliver BMP-2 gene to bone grafts in peri-implant bone defects. Biomaterials. 2007;28:2772–82. [PubMed: 17339051]
34. Carmeliet P. Mechanisms of angiogenesis and arteriogenesis. Nature Med. 2000;6:389–95. [PubMed: 10742145]
35. Ferrara N, Davis-Smyth T. The biology of vascular endothelial growth factor. Endocr Rev. 1997;18:4–25. [PubMed: 9034784]
36. Fischbach C, Mooney DJ, et al. Polymeric systems for bioinspired delivery of angiogenic molecules. In: Abe A, Albertsson A, Duncan R, Dusek K, de Jeu W, Joanny J, editors. Advances in Polymer Science. Vol. 203. Berlin, Heidelberg: Springer; 2006. pp. 191–221.37. Crisan M, Yap S, Casteilla L, Chen CW, Corselli M, Park TS, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell.2008;3:301–13. [PubMed: 18786417]
38. Meyer U, Joos U, Mythili J, Stamm T, Hohoff A, Fillies T, et al. Ultrastructural characterization of the implant/bone interface of immediately loaded dental implants. Biomaterials. 2004;25:1959–67. [PubMed: 14738860]
39. Davies JE, Chernecky R, Lowenberg B, Shiga A. Deposition and resorption of calcified matrix in vitro by rat bone marrow cells. Cells Mater. 1991;1:3–15.
40. Davies JE, Nagai N, Takeshita N, SmithDC. The Bone-Biomaterial Interface. Toronto: University of Toronto Press; 1991. Deposition of cement-like matrix on implant materials; pp. 285–94.
41. Davies JE. in vitro modeling of the bone/implant interface. Anat Rec. 1996;245:426–45. [PubMed: 8769677]
42. Listgarten MA. Soft and hard tissue response to endosseous dental implants. Anat Rec. 1996;245:410–25. [PubMed: 8769676]
43. Raghavendra S, Wood MC, Taylor TD. Early wound healing around endosseous implants: A review of the literature. Int J Oral Maxillofac Implants.2005;20:425–31. [PubMed: 15973954]
44. Davies JE. Understanding peri-implant endosseous healing. J Dent Educ. 2003;67:932–49. [PubMed: 12959168]