A consensus on the limitations of vertical bone augmentation
Vertical augmentation is a dental surgical procedure used to increase the height of the alveolar bone, typically in preparation for dental implant placement. It is needed when there is insufficient bone height in the jaw to support implants, often due to bone loss from conditions such as periodontal disease [1].
Most clinicians emphasize that in vertical bone augmentation, distinguishing between intrabony and extrabony defects is crucial. Intrabony defects, being within the bony contour, are more predictable to reconstruct due to their regenerative capacity and better soft-tissue coverage. Techniques like block bone grafting and guided bone regeneration (GBR) are employed, yet no single method is universally superior [2]. The choice of technique and graft material often depends on the extent of bone gain required, with smaller augmentations achieved through various methods and larger ones typically needing autogenous bone [3]. Vertical bone augmentation is acknowledged as a complex and sensitive surgical procedure with considerable risks, requiring skilled and experienced clinicians.
Stability over time is a key concern with vertical bone grafts in dental surgery [4]. The long-term maintenance of the augmented bone is crucial for successful outcomes. Techniques like GBR and onlay bone grafting have shown favorable results in maintaining bone volume post-surgery. Onlay bone grafts offer specific advantages including avoidance of the inferior alveolar nerve (IAN), ease of placement of the graft, and immediate postoperative vertical augmentation [5]. However, this aspect of bone graft stability is complex and influenced by various factors, including the surgical technique used, the materials chosen for grafting, and individual patient characteristics. Despite immediate benefits, ensuring stability is essential for the overall success and longevity of the augmentation procedure.
Particulate bone with membrane coverage offers both vertical and horizontal mandible augmentation. The membrane prevents connective tissue infiltration, promoting bone formation. This method, however, is technically challenging and risks premature membrane exposure. Metallic mesh, used for vertical ridge augmentation, forms and retains a particulate graft, yielding predictable bone formation if not exposed early [6]. However, mesh exposure during healing can necessitate removal, affecting the augmentation outcome. Both methods require expertise for successful results and have specific complications like membrane or mesh exposure impacting their effectiveness. Achieving a passive, tension-free flap closure over the graft is also crucial, ensuring adequate blood supply and reducing the risk of wound dehiscence. In addition to graft stability and a tension-free flap, clinicians agree incision design, site preparation and maintenance are critical elements of a successful procedure, again emphasizing the need for skilled clinicians.
Retreatment of failed augmentations is notably less predictable [7]. The use of short implants is highlighted as an effective alternative in certain cases, potentially eliminating the need for extensive augmentation. Achieving esthetic results in the anterior maxilla is particularly challenging, often necessitating reliance on dental prosthetics for a natural appearance.
Patient-specific factors, such as compliance, smoking, and health status, significantly influence outcomes. A very thorough risk assessment should be performed to determine if a patient is a good candidate for the procedure.
Vertical augmentation is a complex procedure that necessitates careful risk assessment and the selection of a suitable protocol, material, and therapeutic sequence. Clinicians must evaluate their own expertise and the patient’s appropriateness for the procedure. If these factors are not favorable, alternative methods to vertical ridge augmentation should be considered. This approach ensures both the safety and effectiveness of the treatment.
References:
- Plonka, A.B.; Urban, I.A.; Wang, H.-L. Decision Tree for Vertical Ridge Augmentation. International Journal of Periodontics & Restorative Dentistry 2018, 38.
- Andre, A.; Ogle, O.E. Vertical and horizontal augmentation of deficient maxilla and mandible for implant placement. Dental Clinics 2021, 65, 103-123.
- Misch, C.M.; Basma, H.; Misch-Haring, M.A.; Wang, H.-L. An Updated Decision Tree for Vertical Bone Augmentation. International Journal of Periodontics & Restorative Dentistry 2021, 41.
- Pesce, P.; Menini, M.; Canullo, L.; Khijmatgar, S.; Modenese, L.; Gallifante, G.; Del Fabbro, M. Radiographic and histomorphometric evaluation of biomaterials used for lateral sinus augmentation: A systematic review on the effect of residual bone height and vertical graft size on new bone formation and graft shrinkage. Journal of clinical medicine 2021, 10, 4996.
- Romanos, G.E. Severe Atrophy of the Posterior Mandible and Inferior Alveolar Nerve Transposition. International Journal of Periodontics & Restorative Dentistry 2021, 41.
- Xie, Y.; Li, S.; Zhang, T.; Wang, C.; Cai, X. Titanium mesh for bone augmentation in oral implantology: current application and progress. International journal of oral science 2020, 12, 37.
- Oh, S.-L.; Shiau, H.J.; Reynolds, M.A. Survival of dental implants at sites after implant failure: A systematic review. The Journal of prosthetic dentistry 2020, 123, 54-60.
For more info :
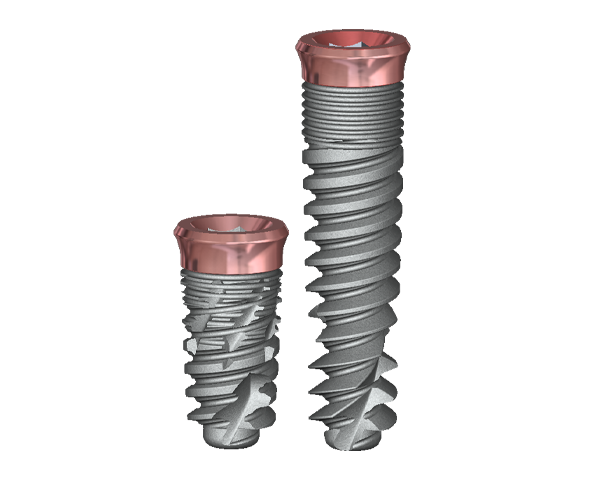
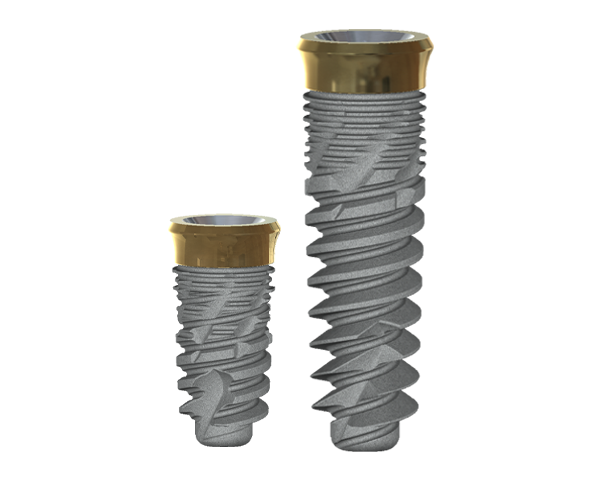
The coated neck of the implant is antibacterial and prevents the formation of biofilms.
State-of-the-art nitriding of titanium allows increases in the depth of nitrogen diffusion, therefore increasing soft tissue adhesion.
The attachment of soft tissue, peri-implant mucosa, surrounding a dental implant creates a seal and is composed of epithelial and connective tissue.
The tissue-level design provides for a more stable seal.