The Biological Implants
Dentalis Bio Solutions’ Research and Development team is a global leader in the research and detection of protein-hormone-growth factor interactions and applications.
We are focused on launching a biological implant. The use of specific growth factors on Dentalis’ implants will improve the prognosis of implantation in sites of low-density bone significantly shortening healing time, contributing to higher success rates of implantation (especially)during immediate loading), and providing excellent aesthetic results.
Here is some extended about growth factor interactions:
Parathyroid hormone 1–34 enhances titanium implant anchorage in low-density trabecular bone: A correlative micro-computed tomographic and biomechanical analysis
Yankel Gabet a, Ralph Müller b, Jay Levy c, Richard Dimarchi c, Michael Chorev d, Itai Bab a,⁎, David Kohavi e
a Institute for Biomedical Engineering, Swiss Federal Institute of Technology (ETH) and University of Zürich, Zürich, Switzerland
b Department of Chemistry, Indiana University, Bloomington, IN 47405, USA
c Laboratory for Translational Research, Harvard Medical School, Cambridge, MA 02115, USA
Internal titanium implants have become the treatment norm in orthopedics and dentistry; however, the efficiency of the implantation process is reduced in low-density bone, and experimental studies show that implant anchorage is hindered after gonadectomy-induced bone loss. The leading anabolic agent used for bone therapy is human parathyroid hormone 1-34 [iahPTH(1-34)], which is administered intermittently; therefore, in this study, Gabet et. al assessed whether iahPTH(1-34) treatment can enhance the integration of titanium implants in low-density bone. Titanium implants with 0.9 mm diameter were implanted horizontally in the proximal zone of the tibial metaphysis of 5-month-old rats seven weeks after they underwent orchiectomy (ORX). iahPTH(1-34) was injected subcutaneously at 5, 25, and 75 µg/kg/day, beginning immediately after the implants were inserted and then administered continuously for the next 8 weeks. The site of implantation was analyzed with µCT at a resolution of 15 µm. The osseointegration (OI) was evaluated and calculated as the percent of the implant surface in touch with bone (%OI). In addition, the volume density of trabecular bone (BV/TV), trabecular thickness (Tb. Th), trabecular number (Tb. N), and connectivity density (Conn.D) were calculated in the peri-implant bone. In ORX rats treated with iahPTH(1-34) the maximal values of %OI, BV/TV, and Tb. The near the implant insertion site was higher than those measured in untreated ORX rats. The biomechanical parameters of the implants from treated rats also exceeded those from the untreated controls, in a dose-dependent manner. Apart from BV/TV and Tb. Th, no significant differences were observed between the different iahPTH(1-34) doses. These findings show that iahPTH(1-34) encourages implant anchorage in bones with low density, suggesting a clinical benefit in administrating iahPTH(1-34) in order to improve the prognosis of implantation in sites of low-density bone.

To download Full Article press here:
Endosseous Implant Anchorage Is Critically Dependent on Mechanostructural Determinants of Peri-Implant Bone Trabeculae
Yankel Gabet,1 David Kohavi,2 Romain Voide,3 Thomas L. Mueller,3 Ralph Mu¨ ller ,3 and Itai Bab1
Institute for Biomechanics, ETH Zu¨ rich, Switzerland
Low bone density is a common issue for patients receiving orthopedic or dental implants, leading to poor implantation prognosis. However, not much is known about the mechanostructural factors that affect implant anchorage. In this study, Gabet et. al demonstrates the importance of the peri-implant bone (PIB) to the anchorage of the implant, using a model of metabolically-induced bone loss. Titanium implants were horizontally implanted into the proximal tibial metaphysis of adult rats six weeks after they underwent orchiectomy (ORX), as well as a group of control rats. Immediately after implantation, the rats were injected with human parathyroid hormone (1-34) [iahPTH(1-34)] or vehicle for six weeks. The implants and bones were then removed and subjected to image-guided failure assessment in order to evaluate the microstructural deformation and biomechanical properties. The failure of anchorage occurred mostly in the PIB trabeculae, 0.5-1.0 mm from the surface of the implant. The anchorage had poorer biomechanical properties in ORX rats with low bone density, mainly due to the decrease in trabecular number. iahPTH(1-34) increased the trabecular thickness (Tb. Th) and therefore rescued the density of the PIB and the mechanical qualities; however, the biomechanical characteristics of the implant were relatively insensitive to treatment that affected the implant surface in low-density bone. These findings further support the model in which the failure of anchorage starts with the weakest trabecular struts, followed by the collapse of the stronger trabeculae. iahPTH(1-34) treatment induced thicker trabecular struts, which delayed and sometimes even prevented the buckling, leading to failure, of the individual elements. Therefore, increasing the trabecular thickness is a prime target for improving implant anchorage by systemic bone anabolic therapy.

Yankel Gabet,1 David Kohavi,2 Romain Voide,3 Thomas L. Mueller,3 Ralph Mu¨ ller ,3 and Itai Bab1
Institute for Biomechanics, ETH Zu¨ rich, Switzerland
Low bone density is a common issue for patients receiving orthopedic or dental implants, leading to poor implantation prognosis. However, not much is known about the mechanostructural factors that affect implant anchorage. In this study, Gabet et. al demonstrates the importance of the peri-implant bone (PIB) to the anchorage of the implant, using a model of metabolically-induced bone loss. Titanium implants were horizontally implanted into the proximal tibial metaphysis of adult rats six weeks after they underwent orchiectomy (ORX), as well as a group of control rats. Immediately after implantation, the rats were injected with human parathyroid hormone (1-34) [iahPTH(1-34)] or vehicle for six weeks. The implants and bones were then removed and subjected to image-guided failure assessment in order to evaluate the microstructural deformation and biomechanical properties. The failure of anchorage occurred mostly in the PIB trabeculae, 0.5-1.0 mm from the surface of the implant. The anchorage had poorer biomechanical properties in ORX rats with low bone density, mainly due to the decrease in trabecular number. iahPTH(1-34) increased the trabecular thickness (Tb. Th) and therefore rescued the density of the PIB and the mechanical qualities; however, the biomechanical characteristics of the implant were relatively insensitive to treatment that affected the implant surface in low-density bone. These findings further support the model in which the failure of anchorage starts with the weakest trabecular struts, followed by the collapse of the stronger trabeculae. iahPTH(1-34) treatment induced thicker trabecular struts, which delayed and sometimes even prevented the buckling, leading to failure, of the individual elements. Therefore, increasing the trabecular thickness is a prime target for improving implant anchorage by systemic bone anabolic therapy.

To download Full Article press here:
Trabecular Bone Gradient in Rat Long Bone Metaphyses: Mathematical Modeling and Application to Morphometric Measurements and Correction of Implant Positioning
Yankel Gabet,1,2 David Kohavi,3 Thomas Kohler,2 Mario Baras,4 Ralph Müller,2 and Itai Bab1
Institute for Biomedical Engineering, University and ETH Zu¨ rich, Zu¨ rich, Switzerland; 3Oral Implant Center, Department of Prosthodontics,
The metaphyseal trabecular bone of mammals is distributed in an uneven manner, so it is necessary to define a standard reference volume in order to enable proper analyses of metaphyseal sites. In this research, conducted by Gabet et. al, the metaphyses of tibias and femurs from orchiectomies (ORX) rats and control rats were scanned and analyzed by µCT six weeks after the operation. 3D images were retrieved and morphometric analysis was conducted using curve-fit analysis. The same process was carried out for proximal tibial metaphyseal sites into which titanium implants were inserted horizontally 6 weeks after the ORX operation and examined 2-12 weeks after the implantation was performed. The curve-fit analysis of the femur and tibia demonstrated a similar decrease for all the morphometric parameters that were examined for both ORX and controls, but the ORX rats showed lower values. For the bone volume (BV/TV) and connectivity densities (Conn.D), the effect of the ORX increased towards the area of the diaphysis. The number of trabeculae was unaffected, and the trabecular thickness decreased in the femur but did not change in the tibia. These findings should prove important for morphometric studies for the determination of reference volumes.
To download Full Article press here:
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing
the risk of peri-implant disease. The enhanced deep thread
simplifies the insertion and allows for high primary stability.
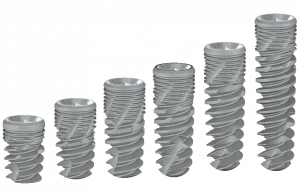
A wide variety of implant systems are offered in order to
suit the widest range of bone densities. Our technologies
are constantly being updated to offer a range of parts that
allow the flexibility that is vital to achieving the most
aesthetically pleasing results.
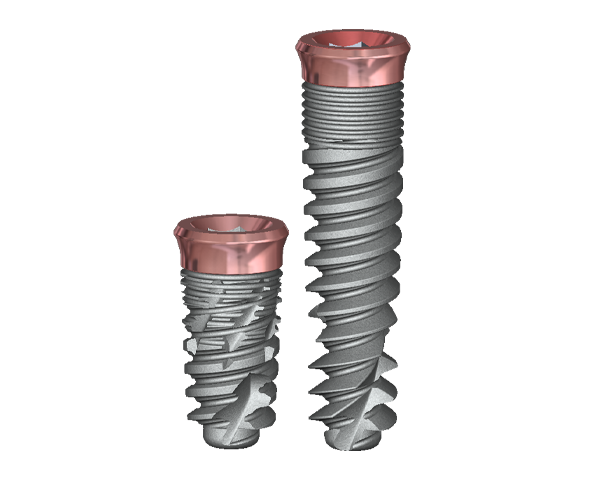
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease. The enhanced deep thread simplifies the insertion and allows for high primary stability.
A wide variety of implant systems are offered in order to suit the widest range of bone densities. Our technologies are constantly being updated to offer a range of parts that allow the flexibility that is vital to achieving the most
aesthetically pleasing results.

Stay Safe. Wear a Mask!
The pink tissue versatile implant neck combines superior gingival aesthetics and high primary stability, improved placement, and temporization,
which is particularly beneficial in
aesthetically demanding cases.
The pink tissue versatile implant neck combines superior gingival aesthetics and high primary
stability, improved placement, and
temporization, which is particularly
beneficial in aesthetically demanding
cases.
The pink tissue versatile implant neck combines superior gingival aesthetics and high primary stability, improved placement, and temporization, which is particularly beneficial in aesthetically demanding cases.