In vivo study with Dentalis Surface
Purpose
To determine the in vivo behavior of titanium alloy implants using bone-to-implant contact (BIC) and torque removal force. Implant Characterization.
The implant surfaces were produced as described: The control implants were rolled smooth surfaces; the rough implants were smooth implants that were grit-blasted with Hydroxy-Apatite/Beta-tricalcium phosphate to reach micron-scale roughness of 3.3μm.
The morphology of the implant surfaces was examined by
scanning electron microscopy, and surface chemical
composition was analyzed by XPS and EDX.
In vivo study with Dentalis Surface
Purpose
To determine the in vivo behavior of titanium alloy implants
using bone-to-implant contact (BIC) and torque removal
force. Implant Characterization.
The implant surfaces were produced as described:
The control implants were rolled on smooth surfaces;
the rough implants were smooth implants that
were grit-blasted with Hydroxy-Apatite/Beta-tricalcium
phosphate to reach micron-scale roughness
of 3.3μm.
The morphology of the
implant surfaces was
examined by scanning
electron microscopy, and
surface chemical
composition was
analyzed by XPS
and EDX.
In vivo model
The sheep model was chosen because of its similarities with humans in anatomy, size, and material and biomechanical characteristics.
The study was approved by the Committee for the Supervision of Animal Experiments. Fifteen healthy female adult sheep weighing between 59 and 75 kg were randomly assigned to one of two treatment groups. Eight sheep received smooth implants and seven sheep received rough implants.
This number of sheep was based on a power analysis, which indicated that this is the smallest number of animals that would allow the detection of significant differences. Each ewe received four implants, all of the same type. Fusion rods were connected vertically to the implants in order to achieve fixation and allow the implants to be load-bearing. Bone chips were grafted as needed.
Radiographs were obtained under general anesthesia to evaluate the placement of the implants.

In Vivo Assessment of Implant success
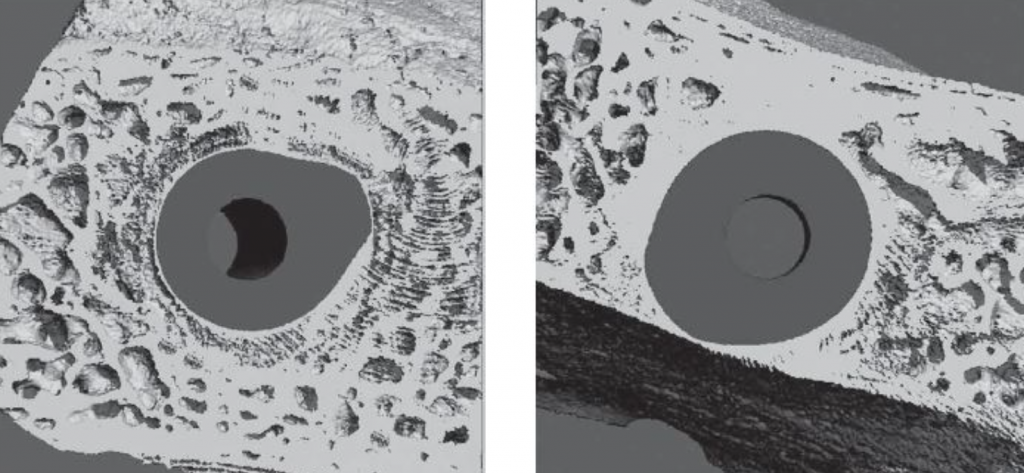
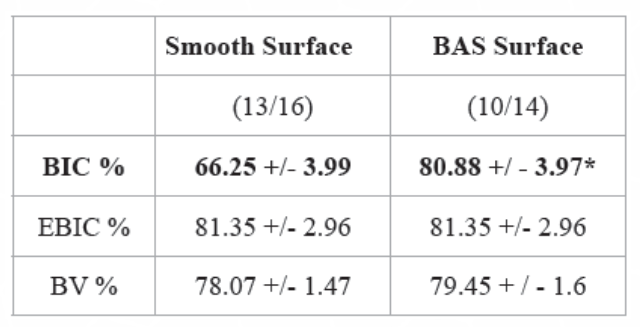
Micro-CT analysis Peri-implant bone formation was seen for both smooth and grit-blasted screws.
More bone attachment to Dentalis implant surface with the 3.3 was noted in the rough surfaces. (Figure 9)
μCT of implants (Smooth surface, Left panel; BAS Surface-Dentalis, right panel).
Histology and Histomorphometry
Tissue sections were prepared from plastic-embedded formalin-fixed tissue blocs with the implant intact.
These sections were ground to a final thickness of 10 to 20μm. Sections were stained with hematoxylin and eosin for qualitative histology.
The percentage of bone-to-implant contact was measured as the fractional, linear extent of bone opposed to the implant surface divided by the total surface perimeter of the implant. We also calculated the expected percentage of bone-to-implant contact, which is the theoretical amount of bone-to-implant contact for the specific bone volume analyzed. An image of the implant profile was superimposed onto the surrounding bone at three locations: 150, 500, and 1000μm lateral to the original implant surface. The actual percent of bone-to-implant contact was measured at each site, and the mean percent of bone-to-implant contact was calculated. In addition, we measured bone volume percent, which is the percentage of mineralized bone in the total tissue volume.
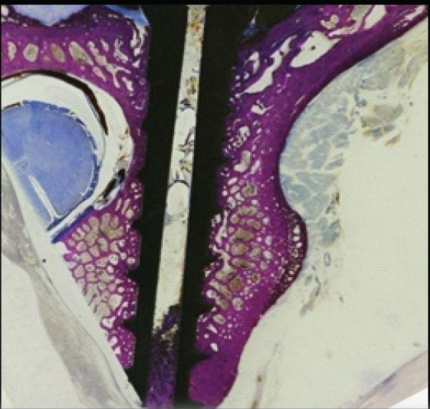
Histology and Histomorphometry
Tissue sections were prepared from plastic-embedded formalin-fixed tissue blocs with the implant intact.
These sections were ground to a final thickness of 10 to 20μm. Sections were stained with hematoxylin and eosin for qualitative histology.
The percentage of bone-to-implant contact was measured as the fractional, linear extent of bone opposed to the implant surface divided by the total surface perimeter of the implant. We also calculated the expected percentage of bone-to-implant contact, which is the theoretical amount of bone-to-implant contact for the specific bone volume analyzed. An image of the implant profile was superimposed onto the surrounding bone at three locations: 150, 500, and 1000μm lateral to the original implant surface. The actual percent of bone-to-implant contact was measured at each site, and the mean percent of bone-to-implant contact was calculated. In addition, we measured bone volume percent, which is the percentage of mineralized bone in the total tissue volume.
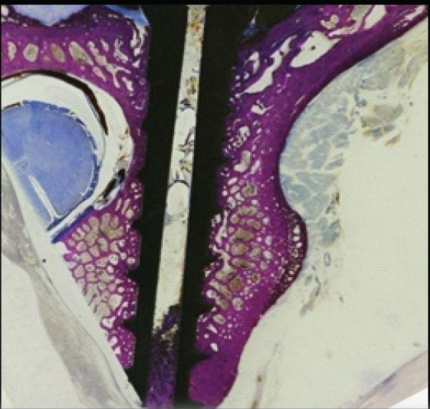
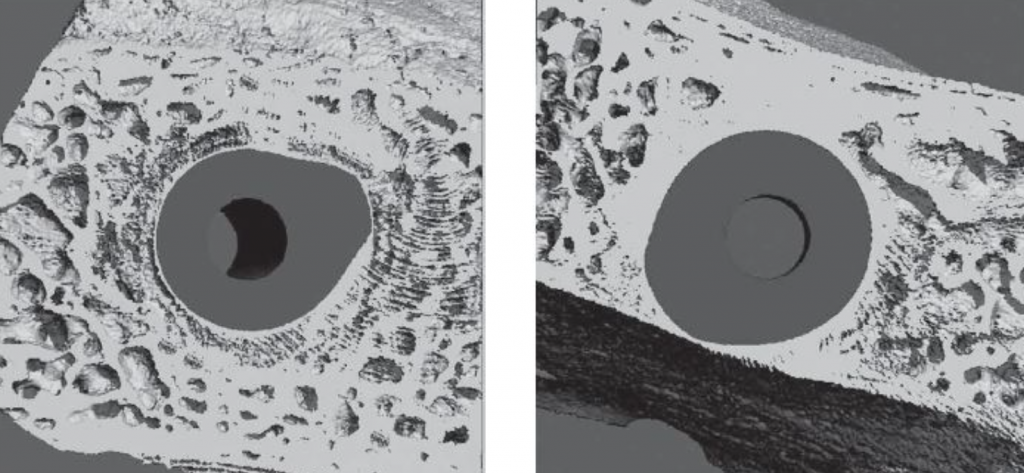
In-vivo experiments also confirmed the advantage of micro-topography of the implant surface in terms of osteoblast growth, adhesion, and mineralized matrix production. Although some bone was formed on the smooth surface implants, it was also covered with fibrous tissue (Fig. 3-a,b,c), which was detached from the surface during the histological processing.

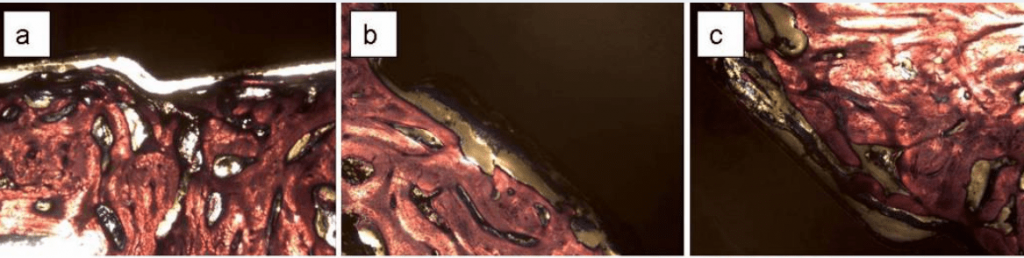
Some fibrous tissue was found also on roughened surfaces (Fig. 3-d,e,f), but it was thinner and more attached to the surface so the detachment was mostly within the bone rather than at the bone-implant interface.
Bone cells were directly attached to the rough surfaces and produced a mineralized matrix.

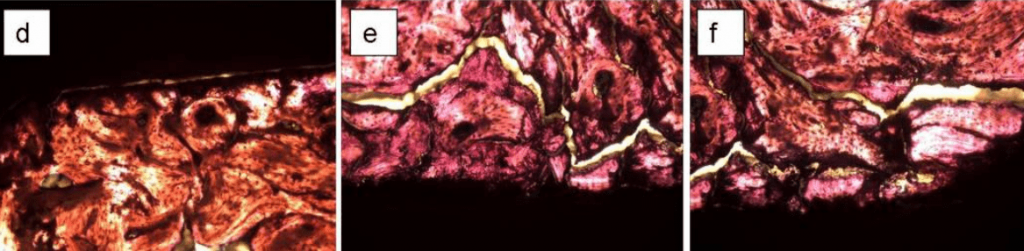
Fig. 3: histological sections oh bone formed on Ti6Al4V pedicle screws implanted in the L4 vertebra of sheep. The screws had smooth (a,b,c) while (c,d,e) rough surfaces with Dentalis 3.3µm
Figure 11:
Undecalcified histology of peri-implant bone formation following osteointegration of smooth (a,b,c) and rough (d,e,f)
Ti6Al4V pedicle screws in the L4 vertebra of sheep.
No magnification (1:1); sections were stained with haematoxylin and eosin
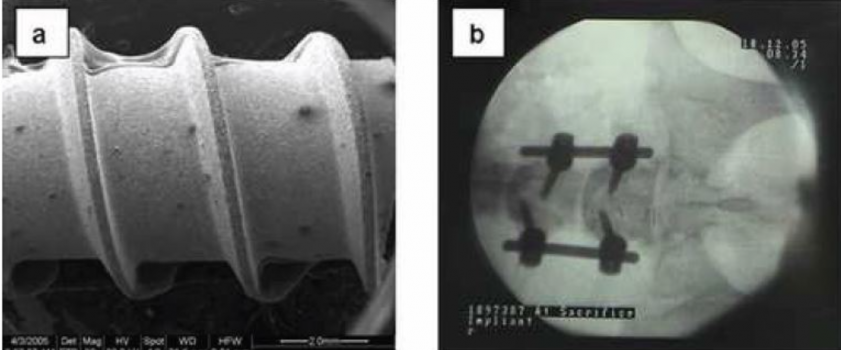
Figure 12:
In vivo assessment of osteointegration.
Panel A: Macrostructure of grit blasted pedicle screw is shown by SEM (x 20).
Panel B: Pedicle screw positions are confirmed by X-ray after implantation. Pedicle screws were inserted into the pedicular notch of L4 & L5 within the vertebral body.
Fusion rods were connected vertically in order to achieve fixation and load-bearing.
Figure 13:
μCT of pedicle screws in the L4 vertebral bone of sheep.
Machined (a-c) or BAS Surface grit blasted (d-f) pedicle screws.
Histology demonstrated that bone formation was not continuous around the implants, but the degree of bone formation was surface-dependent. Although some bone contact was seen on the smooth surfaces, contact areas were also covered by fibrous tissue. Most of the rough surface was covered with bone with a high bone contact area. These histologic observations were supported by histomorphometric measurements.
The average bone-to-implant contact was greater for the grit-blasted screws (73.5% v. 59.6%) (Table 1) (p < 0.05). No differences in bone volume or expected bone-to-implant contact were found.
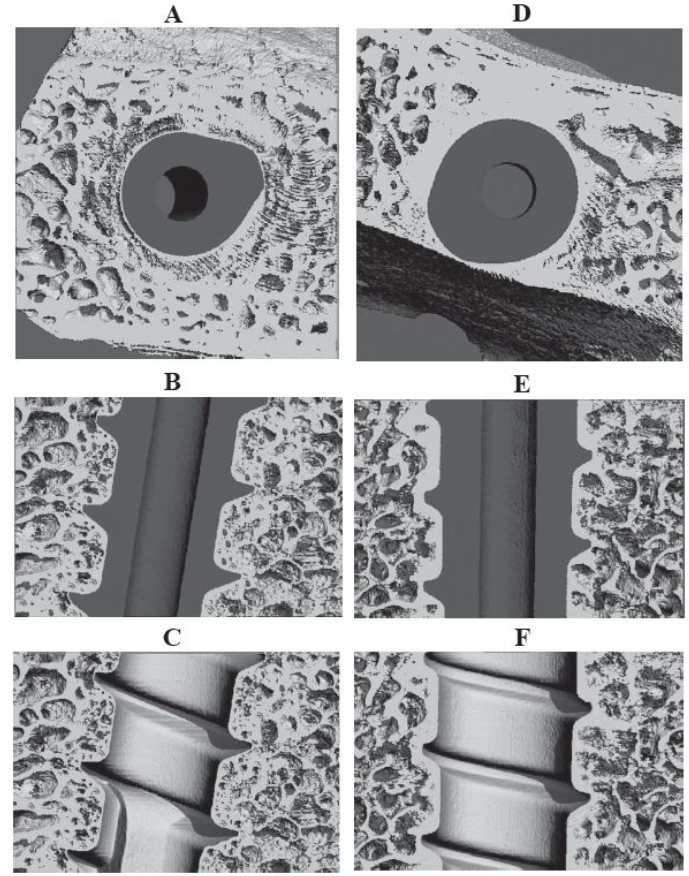
Figure 12:
In vivo assessment of osteointegration.
Panel A: Macrostructure of grit blasted pedicle screw is shown by SEM (x 20).
Panel B: Pedicle screw positions are confirmed by X-ray after implantation. Pedicle screws were inserted into the pedicular notch of L4 & L5 within the vertebral body.
Fusion rods were connected vertically in order to achieve fixation and load-bearing.
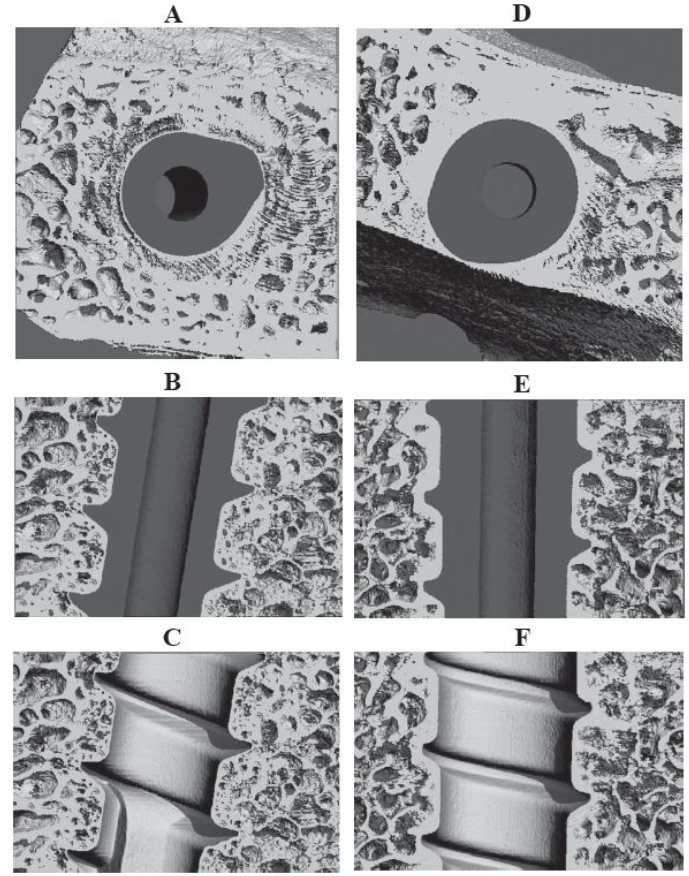
Figure 13:
μCT of pedicle screws in the L4 vertebral bone of sheep.
Machined (a-c) or BAS Surface grit blasted (d-f) pedicle screws.
Histology demonstrated that bone formation was not continuous around the implants, but the degree of bone formation was surface-dependent. Although some bone contact was seen on the smooth surfaces, contact areas were also covered by fibrous tissue. Most of the rough surface was covered with bone with a high bone contact area. These histologic observations were supported by histomorphometric measurements.
The average bone-to-implant contact was greater for the grit-blasted screws (73.5% v. 59.6%) (Table 1) (p < 0.05). No differences in bone volume or expected bone-to-implant contact were found.
Table 3:
Percent bone-to-implant contact (BIC%) of osseointegrated Ti6Al4V pedicle screws implanted for 12 weeks in L4 and L5 vertebrae of sheep spine. 14 of 16 smooth implants and 11 of 14 grit-blasted implants were osseointegrated. The expected bone-to-implant contact percent (EBC%) was defined as the theoretical amount of bone-to-implant contact for the specific bone volume analyzed. The bone volume percent (BV%) is the percentage of mineralized bone in the total tissue volume. Data are means ± SEM. *p
The mean Bone Implant Contact (BIC%), Expected Bone Contact ( EBC % ), and Corresponding Bone Volume (BV%)
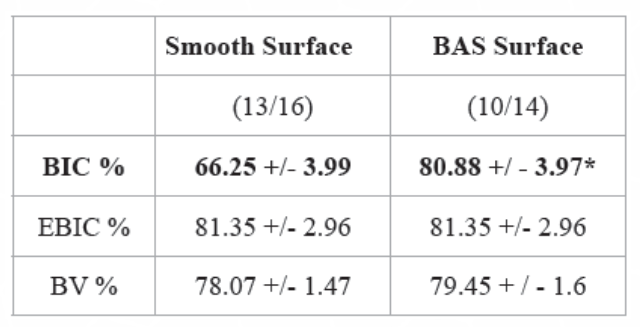
Table 3:
Percent bone-to-implant contact (BIC%) of osseointegrated Ti6Al4V pedicle screws implanted for 12 weeks in L4 and L5 vertebrae of sheep spine. 14 of 16 smooth implants and 11 of 14 grit-blasted implants were osseointegrated.
The expected bone-to-implant contact percent (EBC%) was defined as the theoretical amount of bone-to-implant contact for the specific bone volume analyzed. The bone volume percent (BV%) is the percentage of mineralized bone in the total tissue volume. Data are means ± SEM. *p
The mean Bone Implant Contact (BIC%), Expected Bone Contact ( EBC % ), and Corresponding Bone Volume (BV%)
Each data is the mean +/- SEM
* Significant differences Vs.rough
( ) The number of implant measured / The number of implant inserted
Mechanical Testing
Removal torque measurements were made using a calibrated MTS 858 Mini Bionix II testing system
(MTS Corp, Minneapolis, MN).
The torque angle and moments were recorded automatically with a Test star data acquisition
system.
From the torsion tests, the maximum torque and
angle stiffness was calculated.
The maximum torque was defined as the
removal torque. (Figure 13)
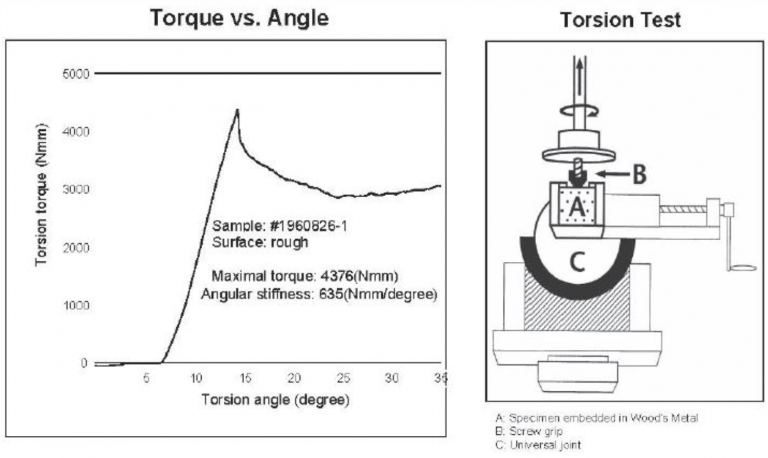
Mechanical Testing
Removal torque measurements were made using a calibrated MTS 858 Mini Bionix II testing system
(MTS Corp, Minneapolis, MN).
The torque angle and moments were recorded automatically with a Test star data acquisition
system.
From the torsion tests, the maximum torque and
angle stiffness was calculated.
The maximum torque was defined as the
removal torque. (Figure 13)
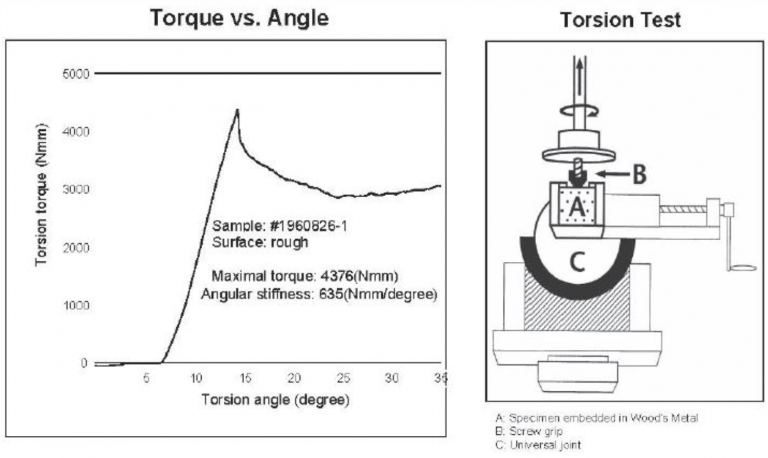
Figure 14:
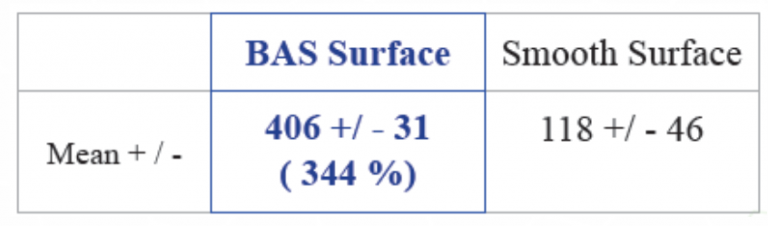
Representative example for graph assessing removal torque of pedicle screws in sheep spine apparatus. Removal torque measurements also showed a statistically significant surface-dependent difference in the mechanical strength of the osseointegration.
BAS Surface ( Dentalis )Grit-blasted pedicle screws required 4061±313N.m (N=12) for displacement whereas machined screws required 1181±461 N.m (p < 0.0001, N=16). (Table 2)
Table 4: Maximal removal tourque (N*cm)
Conclusions:
These results indicate that Dentalis implants with a rough surface enhance osseointegration.
These implants have superior mechanical properties in-vivo and can be used clinically
for long-term success.
These results indicate that Dentalis implants with a rough surface enhance osseointegration.
These implants have superior mechanical properties in-vivo and can be used clinically
for long-term success.
References:
- Cochran DL, Schenk RK, Lussi A, Higginbottom FL, Buser D. Bone response to unloaded and loaded titanium implants with a sandblasted and acid-etched surface: a histometric study in the canine mandible. J Biomed Mater Res 1998 Apr;40(1):1-11.
- Fini M, Giavaresi G, Greggi T, Martini L, Aldini NN, Parisini P, et al. Biological assessment of the bone-screw interface after insertion of uncoated and hydroxyapatite-coated pedicular screws in the osteopenic sheep. J Biomed Mater Res A 2003 Jul 1;66(1):176-183
- Recker RR. Bone histomorphometry: Techniques and interpretation. Boca Raton, FL: CRC Press; 2006.
- Trisi P, Lazzara R, Rebaudi A, Rao W, Testori T, Porter SS. Bone-implant contact on machined and dual acid-etched surfaces after 2 months of healing in the human maxilla. J Periodontol 2003 Jul;74(7):945-956
Acknowledgments
The study was conducted in the Department of Biomedical Engineering at Georgia
Research Tech and Emory University -Barbara D. Boyan, Ph.D.
This work was supported by Impliant, Inc and not by Dentalis.
The National Science Foundation (EEC 9731645) and
The National Institutes of Health (AR 052102)
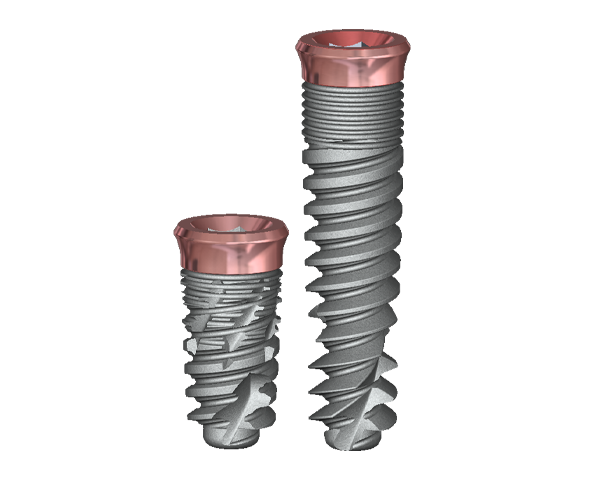
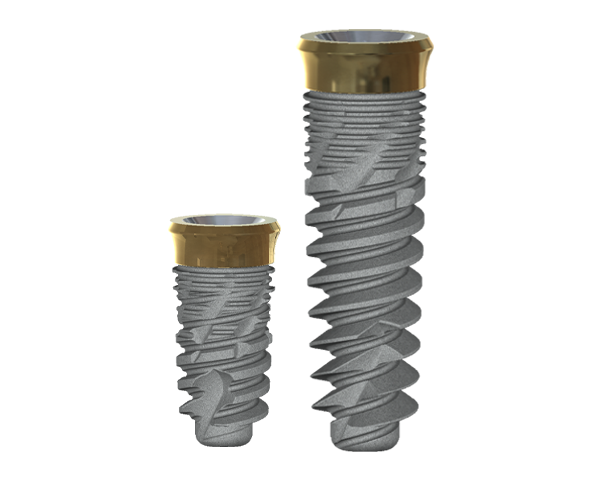
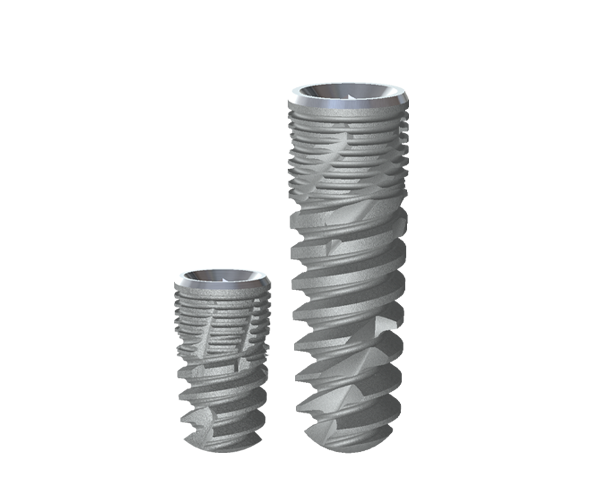
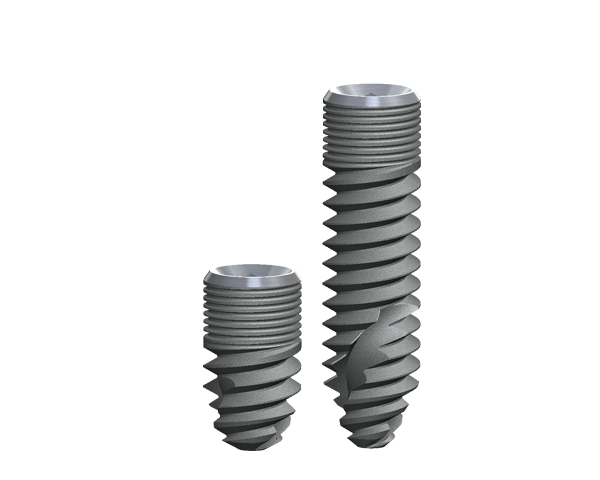
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease.
The enhanced deep thread simplifies the insertion
and allows for high primary stability.
A wide variety of implant systems are offered
in order to suit the widest range of bone densities.
Our technologies are constantly being updated to
offer a range of parts that allow the flexibility that
is vital to achieving the most aesthetically
pleasing results.
The combination of innovative surface technology with 344% stronger bone reduces marginal bone loss and provides for a higher BIC%, decreasing the risk of peri-implant disease. The enhanced deep thread simplifies the insertion and allows for high primary stability.
A wide variety of implant systems are offered in order to suit the widest range of bone densities. Our technologies are constantly being updated to offer a range of parts that allow the flexibility that is vital to achieving the most
aesthetically pleasing results.